What is Skin Cancer?
Skin cancer is a disease in which cancer (malignant) cells are found in the outer layers of your skin. Your skin protects your body against heat, light, infection, and injury. It also stores water, fat and vitamin D.
The skin has two main layers and several kinds of cells. The top layer of skin is called the epidermis. It contains three kinds of cells: flat, scaly cells on the surface called squamous cells; round cells called basal cells; and cells called melanocytes, which give your skin its color.
On this site we provide information on melanoma, basal cell, squamous cell and AK pre-cancers as well as ways to prevent sun damage. This information is not meant in place of a visit to a board-certified dermatologist, but as a supplement to regular screenings.
Actinic Keratosis and Other Precancers
A number of abnormal but relatively harmless skin growths may be precursors of skin cancer. These may be precancerous lesions, benign tumors that mask or mimic more serious ones or malignant tumors that are at the moment just on the topmost layer of the skin. They are important to recognize because they are a warning sign of potential skin cancer.
Precancerous Growths
The term "precancerous" is used because these abnormal areas of skin are more likely to turn malignant than to healthy skin. Precancerous growths (lesions) are visible to the naked eye, and they look different from normal cells when examined under a microscope.
Types of Precancers
Actinic Keratosis - Actinic keratosis (AK), also known as solar keratosis, by far the most common precancer, is the result of prolonged exposure to sunlight. It is a small crusty or scaly bump or horn that arises on or beneath the skin surface. The base may be light or dark, tan, pink, red, or a combination of these or the same color as your skin. The scale or crust is horny, dry and rough, and is often recognized by touch rather than sight. Occasionally it itches or produces a pricking or tender sensation. It can also become inflamed and surrounded by redness. In rare instances, actinic keratoses can bleed.
The skin abnormality or lesion develops slowly and usually reaches a size from an eighth to a quarter of an inch (2mm to 4mm) but can sometimes be as large as one inch. Early on, it may disappear only to reappear later. It is not unusual to see several AKs at a time. AKs are most likely to appear on the face, lips, ears, scalp, neck, backs of the hands and forearms, shoulders and back — the parts of the body most often exposed to sunshine. The growths may be flat and pink or raised and rough.
Actinic keratoses can be the first step leading to sqamous cell carcinoma (SCC). Some studies show that ten percent do advance, and 40-60 percent of SCCS begin as untreated AKs.
Actinic cheilitis - Actinic cheilitis is a type of actinic keratosis or leukoplakia occurring on the lips. It causes them to become dry, cracked, scaly and pale or white. It mainly affects the lower lip, which typically receives more sun exposure than the upper lip.
Leukoplakia - Leukoplakia is a disease of the mucous membrane. White patches or plaques develop on the tongue or inside of the mouth, and have the ability to develop into SCC. It is caused by sources of continuous irritation, including smoking or other tobacco use, rough edges on teeth, dentures or fillings. Leukoplakia on the lips is caused mainly by sun damage.
Bowen's Disease - This is generally considered to be a superficial SCC that has not yet spread. It appears as a persistent red–brown, scaly patch which may resemble psoriasis or eczema. If untreated, it may invade deeper structures.
Arsenical keratosis - Far less common, arsenical keratosis is an accumulation of keratinized tissue that at first resembles numerous small, yellowish corns. These arise most often on the palms, soles and inner surfaces of the finger and toes, and then enlarge and thicken, sometimes increasing in number. Although rarely seen today, arsenical keratoses usually occur on patients who were at some time in their live exposed to arsenic, either contained in medication or from an industrial or environmental source.
Regardless of appearance, any change in a pre-existing skin growth, or the development of a new growth or open sore that fails to heal, should prompt an immediate visit to a physician. If it is a precursor condition, early treatment will prevent it from developing into SCC. Often, all that is needed is a simple surgical procedure or application of a topical chemotherapeutic agent.
Treatment
Treated early, almost all actinic keratoses (AKs) can be eliminated before becoming skin cancer. There are many effective methods for removing AKs, and the choice is determined by many factors, including the location, type and size of the lesion, and also the health, age and preference of the patient and the preference and experience of the physician. For example, a treatment that has a high cure rate and is painless but leaves a large scar might not be preferred for a tumor on the face. Talk with your physician about treatment option here.
BASAL CELL
Basal cell carcinoma (BCC) is the most common form of cancer, with about a million new cases estimated in the U.S. each year. Basal cells line the deepest layer of the epidermis. An abnormal growth, a tumor, in this layer is, therefore, a basal cell carcinoma.
Basal cell carcinoma can usually be diagnosed with a simple biopsy and is fairly easy to treat when detected early. However, 5 to 10 percent of BCCs can be resistant to treatment or locally aggressive, damaging the skin around them, and sometimes invading bone and cartilage. When not treated quickly, they can be difficult to eliminate. Fortunately, however, this is a cancer that has an extremely low rate of metastasis, and although it can result in scars and disfigurement, it is not usually life threatening.
Cause
The sun is responsible for over 90 percent of all skin cancers, including BCCs, which occur most frequently on the sun-exposed areas of the body: face, ears, neck, scalp, shoulders, and back.
Am I at risk?
Anyone with a history of frequent or intermittently intense sun exposure can develop BCC, but a number of factors increase risk.
Time Spent Outdoors - People who work outdoors, construction workers, groundskeepers, lifeguards, etc., are at greater risk than people who work indoors, as are those who spend their leisure hours in the sun.
Skin Type - Fair-skinned individuals who sunburn easily and tan minimally or not at all have a higher incidence of skin cancer than dark-skinned individuals.
Hours of sunlight - The more hours of sunlight in the day, the greater the incidence of skin cancer. For example, there are more cases in Arizona, Texas and Florida, states that are closer to the equator and get more sun, than in the more northern states of Maine, Oregon and Washington.
Warning Signs
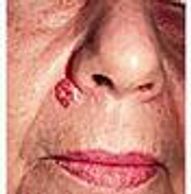
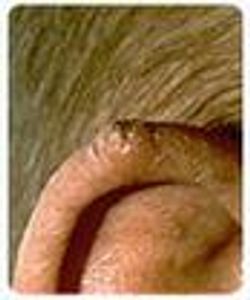
The five most typical characteristics of basal cell carcinoma are shown in the pictures below. Frequently, two or more features are present in one tumor. In addition, BCC sometimes resembles noncancerous skin conditions such as psoriasis or eczema. Only a trained physician can decide for sure. If you observe any of the warning signs or some other change in your skin, consult your physician immediately.
Basal cells
Open Sore
Reddish Patch
Reddish Patch

Open Sore - A sore that bleeds, oozes or crusts and remains open for a few weeks. A persistent, non-healing sore is a very common sign of an early basal cell carcinoma.
Reddish Patch
Reddish Patch
Reddish Patch

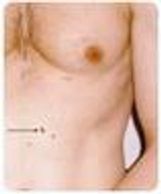
A Reddish Patch - A patch or irritated area, frequently occurring on the chest, shoulders, arms or legs. Sometimes the patch crusts. It may also itch or hurt. At other times, it persists with no noticeable discomfort.
Shiny Bump
Reddish Patch
Pink Growth

A Shiny Bump - A bump or nodule that is pearly or translucent and is often pink, red or white. The bump can also be tan, black or brown, especially in dark-haired people, and can be confused with a mole
Pink Growth
Scar like Area
Pink Growth
A Pink Growth - Slightly elevated rolled border and a crusted indentation in the center. As the growth slowly enlarges, tiny blood vessels may develop on the surface.
Scar like Area
Scar like Area
Scar like Area

A Scar-Like Area - White, yellow or waxy, and often has poorly defined borders. The skin itself appears shiny and taut. This warning sign can indicate the presence of small roots, which make the tumor larger than it appears on the surface.
Types of Basal Cell Carcinomas
Nodular basal cell carcinoma - Most common type. This tumor usually resembles a smooth, round, waxy pimple, pale yellow or pearl gray, and may vary in size from a few millimeters to 1 centimeter. Often, the skin covering the nodule is so thin that the slightest injury will cause it to bleed. These tumors are often depressed in the middle and show ulceration. As the tumor grows, it destroys healthy structures in its path, including nerves, muscles and blood vessels. Large tumors are easily diagnosed, but smaller ones are often difficult to tell from noncancerous skin conditions, such as warts, seborrheic keratoses, moles, and psoriasis.
Superficial - This is a less common form of BCC. It is a progressively spreading, slow-growing cancer that differs greatly from other types. The tumor is red, with a slightly raised, ulcerated or crusted surface, often bordered with pearly or threadlike formations. Tumors usually appear as patches on the torso, but can develop more extensively on the face and neck. This is often mistaken for other skin conditions such as fungal infections, eczema or psoriasis.
Sclerosing or Fibrosing - Fibrosing basal cell carcinoma is also called morphea-like carcinoma. This fibrosing type of tumor begins as a flat or slightly depressed, shiny, hard, yellow-white patch with an irregular border. Sometimes, it may be present for years without growing or being recognized. More often, though, the lesion grows quickly, reaching a diameter of several centimeters within a few months. This is a fairly uncommon type of skin cancer, and can be difficult to eradicate because of invisible root-like extensions of the tumor that reach into the underlying tissue.
Pigmented - Pigmented basal cell carcinoma is similar to nodular basal cell carcinoma, but is more likely to appear in people with dark hair or dark eyes. As its name implies, this growth is almost black and can easily be mistaken for the more aggressive melanoma.
Fibroepithelioma - This is a rare type of basal cell carcinoma appearing as one or more slightly elevated, reddish lesions. Usually they arise on the back.
Basosquamous carcinoma - Squamous and basal cell carcinoma can coexist as one tumor growth at the same time. Clinically, it can look like a basal cell or squamous cell carcinoma. Basosquamous cell carcinomas are believed by some researchers to have a greater tendency to metastasize. These tumors require immediate and aggressive treatment.
Basal cell nevus syndrome - Rarely, basal cell carcinoma may develop as part of an inherited condition, commonly referred to as nevoid basal cell carcinoma syndrome or Gorlin syndrome. Unlike other skin cancer conditions, this syndrome may develop during childhood or adolescence, and as many as 50-100 cancers may be involved. Sometimes, the skin cancers increase in number as the person reaches adulthood. Clinically, they have the same appearance as basal cell carcinomas.
Treatment
The vast majority of BCCs are not serious if detected early and treated quickly. The BCCs that cause trouble are the ones that have been neglected until they have become so thick that they are hard to treat.
There is no one best method to treat all skin cancers and precancers. The choice is determined by many factors, including the location, type and size, whether it is a primary tumor or a recurrent one, the health and preference of the patient, and the physician's experience with the technique. For example, a treatment that has a high cure rate and is painless but leaves a large scar might be acceptable for a tumor on the body, but not on the face.
Almost all treatments can be performed in the physician’s office or in a special surgical facility. Most skin cancer removal can be done using a local anesthetic. Rarely, extensive tumors may require general anesthesia and hospital admission.
Squamous Cell
Squamous cell carcinoma (SCC) is the second most common form of skin cancer, with over 250,000 new cases per year estimated in the U.S.. It arises in the squamous cells that compose most of the upper layer of the skin.
Most SCCs are not serious. When identified early and treated promptly, the future is bright. However, if overlooked, they are harder to treat and can cause disfigurement. While 96 to 97 percent of SCCs are localized, the small percentage of remaining cases can spread to distant organs and become life-threatening.
Cause
Chronic overexposure to the sun is the primary cause of most cases of squamous cell carcinoma. Tumors appear most frequently on the sun-exposed face, neck, bald scalp, hands, shoulders, arms, and back. The rim of the ear and the lower lip are especially vulnerable to these cancers.
SCCs may also occur where skin has suffered certain kinds of injury: burns, scars, long-standing sores, sites previously exposed to X-rays or certain chemicals (such as arsenic and petroleum by-products). In addition, chronic skin inflammation or medical conditions that suppress the immune system over an extended period of time may encourage development of the disease.
Occasionally, squamous cell carcinoma arises spontaneously on what appears to be normal, healthy, undamaged skin. Some researchers believe that a tendency to develop this cancer may be inherited.
Am I at risk?
Anyone with a substantial history of sun exposure can develop squamous cell carcinoma but certain environmental and genetic factors can increase the potential for this disease.
Sun Exposure - Sunlight is responsible for over 90 percent of all skin cancers. Working primarily outdoors, living in an area that gets a lot of high intensity sunlight (like Australia), and spending time in tanning booths all increase your exposure to UV rays and thus increase your risk for developing skin cancer, including squamous cell carcinoma.
Skin Type - People who have fair skin, light hair, and blue, green, or gray eyes are at highest risk. Hispanics, Asians and dark-skinned individuals of African descent are far less likely than Caucasians to develop skin cancer. Check out your skin type and how it affects your skin cancer risk.
Previous Skin Cancer - Anyone who has had a skin cancer of any type is at increased risk of developing another one.
Reduced Immunity - People with weakened immune systems due to excessive unprotected sun exposure, chemotherapy, or illnesses such as HIV/AIDS are more likely to develop squamous cell carcinoma.
Warning Signs
Squamous cell tumors are thick, rough, horny and shallow when they develop. Occasionally, they will ulcerate, which means that the epidermis above the cancer is not intact. There will be a raised border and a crusted surface over a raised, pebbly, granular base.
Any bump or open sore in areas of chronic inflammatory skin lesions indicates the possibility of squamous cell carcinoma, and a doctor should be consulted immediately if this is the case. Usually, the skin in these areas reveals telltale signs of sun damage, such as wrinkling, changes in pigmentation and loss of elasticity. That is why tumors appear most frequently on sun-exposed parts of the body.
Squamous cells
A wart-like growth that crusts and occasionally bleeds.

A persistent, scaly red patch with irregular borders that sometimes crusts or bleeds.

An open sore that bleeds and crusts and persists for weeks.

An elevated growth with a central depression that occasionally bleeds. A growth of this type may rapidly increase in size.
Treatment
The vast majority of SCCs are not serious if detected early and treated quickly. However, squamous cell carcinoma can grow quickly and can be resistant to treatment or locally aggressive, damaging healthy skin around it, sometimes even reaching into bone and cartilage. With delays in treatment, it may be difficult to eliminate, and could result in disfigurement.
Squamous cell carcinomas that are at high risk for metastasis are usually found on the lip, ear, nose, or in persons who are immunocompromised. Speak with your Brevard Skin and Cancer Center physician about your treatment options.
Melanoma
Melanoma is the most serious form of skin cancer. However, if it is recognized and treated early, it is nearly 100 percent curable. But if it is not, the cancer can advance and spread to other parts of the body, where it becomes hard to treat and can be fatal. While it is not the most common of the skin cancers, it causes the most deaths. The American Cancer Society estimates that in 2007, there will be 8,110 fatalities, 5,220 in men and 2,800 in women in the U.S. The number of new cases of melanoma is estimated at 59,940. Of these new cases, 33,910 will be in men and 26,030 in women. Melanoma is a malignant tumor that originates in melanocytes, the cells which produce the pigment melanin that colors our skin, hair and eyes. The majority of melanomas are black or brown. However, some melanomas are skin-colored, pink, red, purple, blue or white.
Am I at risk?
Everyone is at some risk for melanoma, but increased risk depends on several factors: sun exposure, number of moles on the skin, skin type and family history (genetics).
Sun exposure - Both UVA and UVB rays are dangerous to the skin and can induce skin cancer, including melanoma. Blistering sunburns in early childhood increase risk, but cumulative exposure also is a factor. People who live in locations that get more sunlight — like Florida, Hawaii, and Australia — get more skin cancer. Avoid using a tanning booth or tanning bed, since it increases your exposure to UV rays, thus increasing your risk of developing melanoma and other skin cancers.
Moles- There are two kinds of moles: normal moles — the small brown blemishes, growths, or "beauty marks" that appear in the first few decades of life in almost everyone — and atypical moles, also known as dysplastic nevi. Regardless of type, the more moles you have, the greater your risk for melanoma.
Skin Type- As with all skin cancers, people with fairer skin are at increased risk.
Family History- About one in every ten patients diagnosed with the disease has a family member with a history of melanoma. If your mother, father, siblings or children have had a melanoma, you are in a melanoma-prone family. Each person with a first-degree relative diagnosed with melanoma has a 50 percent greater chance of developing the disease than people who do not have a family history. If the cancer occurred in a grandmother, grandfather, aunt, uncle, niece or nephew, there is still an increase in risk, although it is not as great.
Personal History- Once you have had melanoma, you run an increased chance of recurrence. Also, people who have or had basal cell carcinoma and squamous cell carcinoma are at increased risk for developing melanoma.
Weakened Immune System - A compromised immune system resulting from chemotherapy, an organ transplant, excessive sun exposure, and diseases such as HIV/AIDS or lymphoma can increase your risk of melanoma.
Warning Signs: The ABCDEs of Melanoma
Moles, brown spots and growths on the skin are usually harmless — but not always. Anyone who has more than 100 moles is at greater risk for melanoma. The first signs can appear in one or more atypical moles. That's why it's so important to get to know your skin very well and to recognize any changes in the moles on your body. Look for the ABCDEs of melanoma, and if you see one or more, make an appointment with a dermatologist immediately.

Asymmetry- If you draw a line through this mole, the two halves will not match.

Border - The borders of an early melanoma tend to be uneven. The edges may be scalloped or notched.

Color - Having a variety of colors is another warning signal. A number of different shades of brown, tan or black could appear. A melanoma may also become red, blue or some other color.

Diameter- Melanomas usually are larger in diameter than the size of the eraser on your pencil (1/4 inch or 6 mm), but they may sometimes be smaller when first detected.
Evolving - Any change in size, shape, color, elevation, or another trait, or any new symptom such as bleeding, itching or crusting points to danger.

Prompt action is your best protection. The pictures below show atypical normal moles and melanomas.
Types of Melanoma
The basic types of Melanomas fall into four categories. Three of them begin in situ, meaning they occupy only the top layers of the skin and sometimes become invasive; the fourth is invasive from the start. Invasive melanomas are more serious, as they have penetrated deeper into the skin and may have spread to other areas of the body.
Superficial spreading melanoma - By far the most common type, accounting for about 70 percent of all cases. This is the one most often seen in young people. As the name suggests, this melanoma travels along the top layer of the skin for a fairly long time before penetrating more deeply.
The first sign is the appearance of a flat or slightly raised discolored patch that has irregular borders and is somewhat geometrical in form. The color varies, and you may see areas of tan, brown, black, red, blue or white. This type of melanoma can occur in a previously benign mole. The melanoma can be found almost anywhere on the body, but is most likely to occur on the trunk in men, the legs in women, and the upper back in both.
Lentigo maligna- Similar to the superficial spreading type, as it also remains close to the skin surface for quite a while, and usually appears as a flat or mildly elevated mottled tan, brown or dark brown discoloration. This type of in situ melanoma is found most often in the elderly, arising on chronically sun-exposed, damaged skin on the face, ears, arms, and upper trunk. Lentigo maligna is the most common form of melanoma in Hawaii. When this cancer becomes invasive, it is referred to as lentigo maligna melanoma.
Acral lentiginous melanoma - Spreads superficially before penetrating more deeply. It is quite different from the others, though, as it usually appears as a black or brown discoloration under the nails, on the soles of the feet or palms of the hands. It is the most common melanoma in African-Americans and Asians, and the least common among Caucasians.
Nodular melanoma- Usually invasive at the time it is first diagnosed. The malignancy is recognized when it becomes a bump. It is usually black, but occasionally is blue, gray, white, brown, tan, red or skin tone.
The most frequent locations are the trunk, legs and arms, mainly of elderly people, as well as the scalp in men. This is the most aggressive of the melanomas, and is found in 10 to 15 percent of cases.
Treatment
When it comes to the early stages of the disease, the future is bright. Most people with thin, localized melanomas are cured by appropriate surgery. Early detection still remains the best weapon in fighting skin cancer.
More treatments are available for more advanced disease. The cure rate continues to rise. Research has produced a greater understanding of melanoma, leading to the development of new drugs. A Brevard Skin and Cancer Center physician will go over all treatment options with you.